Appearance
Getting the Diagnosis Right
Many people think of diabetes as a catch all diagnosis and have little knowledge of the difference in pathology between the types. Most medics can describe the difference between type 1 and type 2 but those outside of diabetes medicine may not be aware of the growing classfication of types of diabetes. So if you don't know your Type 3c from your Type 2 then this is the article for you.
Why does it matter in critical care?
How we manage stress hyperglycaemia in a person with no history of diabetes should be different to how we manage hyperglycaemia in a person with Type 2 who is normally poorly controlled.
Taking (and documenting) a detailed diabetes history and sending a HbA1c on admission can have a big impact on how we manage these patients, in ICU and on discharge to the ward.
HbA1C
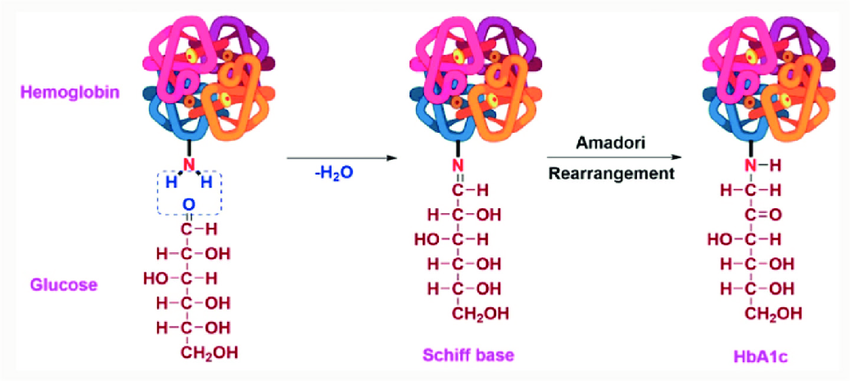
Glycosylated haemoglobin A1c is the standard test for diagnosing diabetes and monitoring effective control. When haemoglobin is exposed to glucose as it normally is in the blood stream, a fraction of it becomes glycosylated (molecules of glucose attach to it). The higher your glucose is for the longer time, the higher your HbA1c is. It is a sensitive marker for average glucose control over the preceeding 2-3 months.
How is it useful in critical care?
We check the HbA1c on admission for all our patients as this has a number of potential benefits
Establishes the diagnosis
When the blood glucose is found to be elevated a few hours or days into the admission it is a useful screening tool to rule in diabetes pre-admission when the pateint is not known to be diabetic. Many things happen during an ICU stay that can cause errors with HbA1c (bleeding, anaemia, tranfusion, fluid resuscitation) so doing this test further into the admission does not add as much value to our diagnosis.
Establish severity / control
Compliance and response to treatment in the community is an important piece of information in guiding management in the ICU but also for planninng management after the patient has recovered and is ready to step down. We recommend a diabetes specialist nurse reviews all our patients with a HbA1c of 60mmol/mol before step down to the ward
HbA1c can give an estimate of the average blood glucose from the preceeding few weeks. Check out this calculator to see how simple this is.
Types of Diabetes
Diabetes can be classified into the following general categories. For an in-depth review of this classification see this article from the American Diabetes Association
- Type 1 diabetes (due to autoimmune β-cell destruction, usually leading to absolute insulin deficiency, including latent autoimmune diabetes of adulthood)
- Type 2 diabetes (due to a progressive loss of adequate β-cell insulin secretion frequently on the background of insulin resistance)
- Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes (such as neonatal diabetes and maturity-onset diabetes of the young), diseases of the exocrine pancreas (such as cystic fibrosis and pancreatitis), and drug- or chemical-induced diabetes (such as with glucocorticoid use, in the treatment of HIV/AIDS, or after organ transplantation)
- Gestational diabetes mellitus (diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation)
As you can see, even in this broad classification of 4 types there are many sub-types and this has an impact on how we manage these patients in hospital and in ICU. A patient with type 2 diabetes managed with diet alone and a HbA1c of 55mmol/mol is likely to have a very different clinical course to someone managed with insulin, an SGLT-2 inhibitor and who has a HbA1c of 95mmol/mol.
How does this change what we do?
The following are cases pickked up on our critical care glucose ward round that highlight how important getting the diabetes diagnosis right can be:
Case 1.
A young woman with no history of diabetes was admitted to the ICU after major abdominal surgery during which she required a splenectomy and distal pancreatectomy. In the days after the operation she developed sepsis and required IV insulin to control her blood glucose. Long acting insulin was started by the diabetes specialist nurse. As she improved her insulin requirements fell and she then started developing hypoglycaemic episodes. Her long acting insulin was reduced and then stopped by the critical care team. A few days later she became unwell and was diagnosed with diabetic ketoacidosis.
What's the diagnosis?
This is type 3c diabetes caused by destruction of the beta cells which can be found in the tail of the pancreas. Typee 3c refers to conditions where diabetes develops after damage to the pancreas from other diseases such as pancreatitis, trauma or as in this case, pancreatectomy.
Whats the relevance to critical care?
This type of diabetes is notoriously difficult to manage as the amount of insulin they require varies dramatically day to day. They are prone to big swings in insulin requirements and often need daily adjustments when unwell. If insulin is stopped they can go into DKA rapidly so a long acting insulin must be continued and regular (sometimes daily) titration by the diabetes team is needed.
Case 2
A 65 year old man is admitted with pneumonia and requires invasive ventilation, steroids and antibiotics. Blood glucose is persistently elevated (12-16mmol/l) for the first few days requiring a variable rate insulin infusion. No previous medical history.
What's the diagnosis?
Not clear unless we look at the HbA1c. This is found to be 95mmol/mol. Review of the history and GP care record show's no history of diabetes. This is a new diagnosis of type 2 diabetes.
What's the relevance to critical care?
This is not simply stress or steroid induced hyperglycaemia and he's not only going to need control in the short term but is likely to benefit from something in the longterm. Starting metformin will help reduce glucose levels but he's likely to need a long acting insulin to reduce the IV insulin need but also in the future. If his HbA1c had been <48mmol/mol this makes type 2 diabetes unlikely and a VRII would be a safer option in the short term.
If a patient in critical care has a history of diabetes or develops hyperglycaemia, take a detailed history including type, duration of diagnosis and medications used to manage pre-admission.
All patients admitted to critical care should have a HbA1C sent to screen for diabetes and establish how well controlled it has been in the community